About us & our product
ImVitro’s SaaS platform EMBRYOLY is an AI-powered software. EMBRYOLY’s core feature provides a ranking based on the embryo’s morphokinetics as well as a subsequent transfer priority recommendation personalized to the patient for increased accuracy. See our product page for more information!
The challenge
Embryo morphokinetics is a key criteria for embryologists to identify the embryo with the highest chance of leading to a pregnancy upon transfer. Embryologists typically rank embryos from good, fair, and poor quality, often discarding poor quality embryos. However, sometimes, only poor quality embryos are available, which can prove even more difficult for embryologists to rank.
Questions to answer
- Can EMBRYOLY’s scores rank poor-quality embryos based on their likelihood of pregnancy?
- How often does EMBRYOLY agree with the embryologist’s choice of first embryo to transfer when patients did get pregnant?
What would have been the impact on the time to pregnancy if the embryologist had transferred EMBRYOLY’s highest ranked embryo?
The study at a glance
1 out of 2
patients left with only poor-quality embryos available for transfer
74%
agreement on highest ranked poor-quality embryo between EMBRYOLY & embryologist for patients who did get pregnant
-2.3 months to pregnancy
if embryologists had transferred EMBRYOLY’s highest ranked poor-quality embryo
Dataset
Data from N=528 patients was acquired through a MIRI® (ESCO) time-lapse system and uploaded on EMBRYOLY from a single center, Centre Sainte Colette at Hôpital Saint-Joseph in Marseille, France, during its initial lab integration between January 2022 and March 2023. In this period, the scores from EMBRYOLY were not necessarily taken into consideration for the final transfer decision. Embryos at day 5, whether they reached blastocysts or not, were identified as poor quality by a separate algorithm built by ImVitro and trained on embryologists’ annotations following the Istanbul grading (Poor, Fair or Good)¹. The data collected was not used in the algorithm’s training described in Human Reproduction².
Findings
Analysing the data uploaded through EMBRYOLY over a year yielded the following insights:
For 47% of the patients (N=204 patients, women's average age 35 y.o.), embryologists were faced with having to choose an embryo to transfer among 4.3±1.7 poor-quality embryos, either because the cohort was composed of only poor-quality embryos from the beginning or because only poor-quality embryos remained after higher quality embryos were transferred first.
A statistically significant increase of +0.02 in EMBRYOLY's score was associated with +2% to +7% relative increase in likelihood of clinical pregnancy (p<0.05, OR = 1.04, 95CI = [1.02-1.07], N=261 transferred embryos), demonstrating EMBRYOLY is able to help embryologists rank amongst poor-quality embryos.
Looking only at patients that did get pregnant, EMBRYOLY’s first choice often agreed with the embryologists’ first choice (in 74% of the cases, N=42 embryos).
Looking only at patients who ended up getting pregnant following multiple cycles (N=28 embryos), EMBRYOLY would have minimized the number of cycles needed to get pregnant by 18%, from 1.7 to 1.4 cycles (McNemar test with continuity correction p<0.05).
EMBRYOLY also agreed with the embryologist’s first choice in 71% of patients who did not get pregnant with their first and only transferred embryo (N=72 embryos). While EMBRYOLY’s highest ranked embryo did not lead to a pregnancy in these cases, it is impossible to know if this is because none of the available embryos would have been able to lead to a pregnancy either.
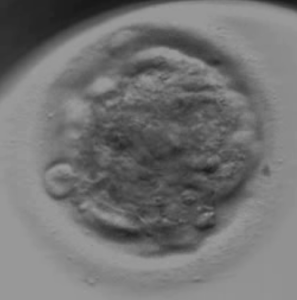
Which one would you have transferred first?
Below are two poor-quality embryos from the same cohort transferred at day 5. Which one would you have transferred first?
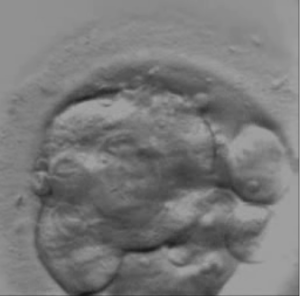
Embryo A
Embryo B
Keep reading to find out the answer! If you want to test out your embryo-ranking skills further, click here.
Conclusion
Embryologists often seem to have to choose between poor-quality embryos. EMBRYOLY can be used as an additional datapoint to help them feel more confident about which poor embryo has the highest chance of leading to a pregnancy.
By reducing the time to pregnancy from 1.7 to 1.4 cycles, EMBRYOLY would have saved an average of 2.3 months of treatment, and allowed the centre to welcome at least 1% additional patients in the same time frame.
This is only part of the picture, as EMBRYOLY could have also helped in the many other cases where the embryologist had to rank good and fair quality embryos.
Contact us to learn how EMBRYOLY can also help with this.
Answer to "which one would you have transferred first?"
Embryo A (scored 0.24) was transferred first but did not lead to a pregnancy. EMBRYOLY ranked first embryo B (scored 0.41), which was transferred second and led to a clinical pregnancy.
¹Alpha Scientists in Reproductive Medicine & ESHRE Special Interest Group of Embryology, 2011