About us & our product
ImVitro’s SaaS platform EMBRYOLY is an AI-powered software. EMBRYOLY’s core feature provides a ranking based on the embryo’s morphokinetics as well as a subsequent transfer priority recommendation personalized to the patient for increased accuracy. See our product page for more information!
The challenge
Ranking embryos is a task that does not increase the inherent chances a patient has to get pregnant with any of their embryos. Rather, it increases the chances of getting pregnant earlier if any of them has the potential to lead to a pregnancy, thus also minimizing the likelihood of dropping out of the treatment. In our latest paper accepted by RBMO, we show that when EMBRYOLY had the opportunity to impact the number of cycles needed to reach a pregnancy (for better or worse), its adjunct use could have shortened it [Dissler et al, 2024]. It is therefore important to acknowledge what portion of patients would realistically benefit from improved ranking provided by EMBRYOLY, and how this would impact the overall success of your clinic.
Questions to answer
- What would have been the impact of EMBRYOLY on the first cycle pregnancy rate (FCP) had it been used as an adjunct tool to the embryologist?
The study at a glance
59±12%
IVF treatments could not be shortened by EMBRYOLY
3
statistically different patient & cohorts characteristics between IVF cycles that could benefit from EMBRYOLY or not
+22±6%
FCP with the adjunct use of EMBRYOLY at the clinic-level
The study at a glance
59±12%
IVF treatments could not be shortened by EMBRYOLY
3
statistically different patient & cohorts characteristics between IVF cycles that could benefit from EMBRYOLY or not
+22±6%
FCP with the adjunct use of EMBRYOLY at the clinic-level
Dataset
Data from 7 French and Spanish clinics were considered for the time period between 2018-2022. Only egg retrievals that had led to at least one transfer with a known outcome were included and oocyte warming cycles were excluded, resulting in N = 2715 egg retrievals. The average maternal age was 35.2±4.9 y.o.
FCP rate was considered as the percentage of egg retrievals that led to a pregnancy following the first embryo transferred; cumulative pregnancy rate (CPR) was considered as the percentage of egg retrievals that led to a pregnancy within one year of the egg retrieval date.
We first quantified the number of patients who could not realistically benefit from EMBRYOLY, as all their usable embryos had been transferred resulting in the same outcome (either never or always getting pregnant, respectively referred to as groups C and B, see figure below). An embryo was considered as “usable” if it had been frozen or transferred by the embryologist.
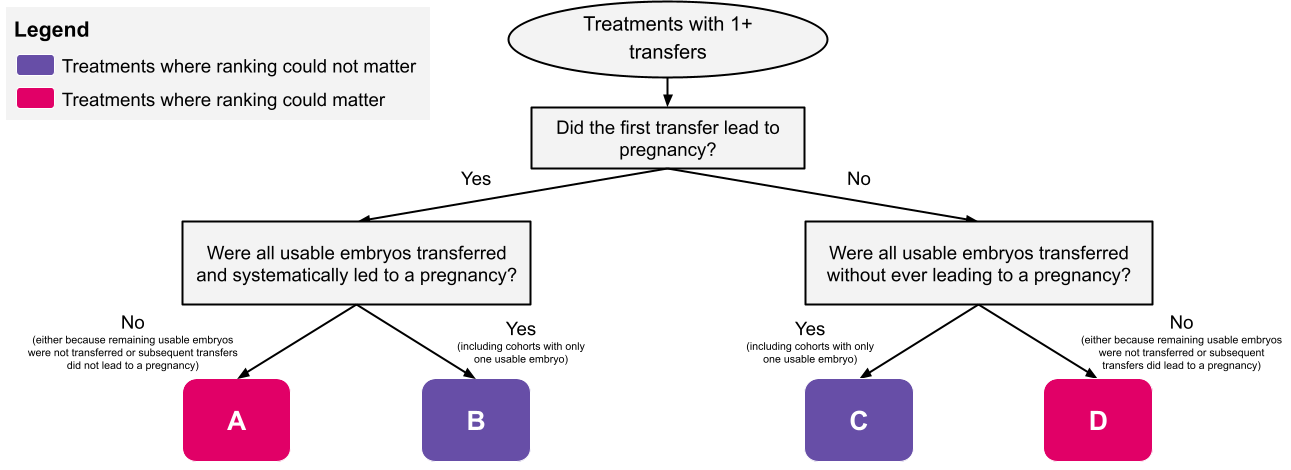
Therefore, we considered that EMBRYOLY could have decreased FCP for couples who got pregnant following the first transfer and had other usable embryos (referred to as group A). Conversely, we considered that EMBRYOLY had the opportunity to increase FCP or CPR for patients who did not get pregnant following the first transfer but still had other usable embryos (referred to as group D) which included drop-out patients, i.e those who did not get pregnant and interrupted their treatment in spite of having remaining frozen embryos. Based on our study published in RBMO, we found that FCP would in these cases be increased on average by 37%.
To quantify and compare embryo quality, we converted the Gardner grade into a linear scale as described by Pierson et al, 2023.
Groups A and D were compared in terms of the patient (maternal age at the time of egg retrieval), the highest embryo quality found in the cohort of sibling embryos and the endometrium thickness of the patient at the time of their first and fresh transfer (thus excluding 14% of the cycles where the first transfer was frozen) using unpaired Student t-tests and multivariate logistic regression.
Findings
Embryo ranking wouldn’t have mattered in 59±12% of IVF treatments per clinic, for which all usable embryos had been transferred and led to the same pregnancy outcome (corresponding to 49±14% treatments where no pregnancy was ever reached and 9 ± 5% where every transfer led to a pregnancy). In contrast, the order of transfer could have mattered for the remaining 41 ± 12% of IVF treatments because they had remaining usable embryos following the first transfer, whether it led to pregnancy (23±6%, group A) or not (18±7%, group D).
When ranking could have mattered, patient age, endometrium thickness at the time of the fresh transfer and quality of the top embryo in the cohort were significantly different between groups A & D (Student t-tests, p < 0.01). Generally, group D showed a combination of older maternal age (+1 y.o), thinner endometrium thickness (-0.7 mm) and lower embryonic quality for the top embryo in the cohort (-0.3 points) when compared to group A (p<0.01, multivariate logistic regression). By entering these three data points together in EMBRYOLY, it could indicate to the user whether it can add value to the ranking of the embryologist for a given cycle (i.e. whether a cycle belongs to group A or D).
+22±6% FCP with the adjunct use of EMBRYOLY for the clinics considered in this dataset, corresponding to an increase in FCP of 7±2 points. This is assuming that EMBRYOLY would impact FCP only in group D, and not group A as follows:
FCPclinic+ImVitro = FCPclinic + 0,37 x %GroupD
On EMBRYOLY, cycles that share the previously described characteristics of group A would be flagged as such to embryologists, who would know not to challenge themselves in such cases.
This relative change in FCP translates into a relative increase in CPR of +11±8%, or an increase of 4 ± 3 CPR points. This corresponds majoritarily to drop-out patients who would have gotten pregnant on their first try thanks to EMBRYOLY because in this dataset, 98% of patients who got pregnant did so within a year of their egg retrieval.
Conclusion at a glance
It is important to acknowledge that not all patients can benefit from improved ranking (whether it is AI-assisted or not), and that their prevalence will vary based on the prognosis of the patients your clinic welcomes. When ranking could matter, it is equally important for embryologists to distinguish between the IVF cycles where they could use the help of an AI tool or not. In particular, this study reminds us that the impact of embryo potential ends where the one of uterus receptivity begins, since endometrium thickness could impact transfer outcome regardless of embryo ranking.
Regardless, shortening time to pregnancy is only part of the value-add of an AI-driven tool such as EMBRYOLY, as it will still support embryologists in evaluating embryos faster regardless of the patient’s prognosis, in generating clinic-wide KPIs and in knowing how to anticipate future fertilizations for poor prognosis patients.